Our Birth Story - The Birth of a Baby and the Birth of a Mom and a Dad
I’ve been cleaning, straightening, arranging, rearranging. Not very well or fast, losing 18 pounds in less than 6 days, and taking medication to lower my blood pressure which makes my heart beat slower are a few of the things making my efficiency low. I’ve also been existing in a severe protein deficit since July. Oh and I birthed a baby a week ago.
See I clean and straighten when I’m nervous or anxious. Just ask my husband how many arguments start with me with my hands in the sink washing dishes or folding laundry. I’m anxious because I still can’t understand how Ben and I got so lucky to bring home a perfect little human. I’m anxious because I feel like somewhere there was a mistake and she isn’t mine and someone or something will come take her. Even if that thing is time…Enjoy it while it lasts, these times go by so fast, I miss newborn snuggles, smells, and sounds so much...all echo my social media, text feeds, and ears right now.
I’m hoping by recalling our birth story I can convince myself we did this. I also don’t want to forget any of these feelings or memories and even though she’s only 7 days old, I already feel so much has happened.
T Minus 5 Days
Friday a week ago I went to the OB for a visit. I’ve been going twice a week since the week of Christmas – since I spent the night in the hospital for elevated blood pressure and migraines.
My blood pressure had slowly been going up over the last 5 days. At home it was still below the ‘danger’ threshold I was given – below the numbers I was told to call 24/7 if they reached. But it was still going up and staying up.
Along the same timeline, my workplace has undergone a huge transition. One full of stress, anxiety, and adjustments. All of this piled on top of the already stressful job we were asked to continue carrying on during the transition. I’d decided to continue working up until I went into labor. But the elevated blood pressure meant they were going to induce me at 37 weeks. This is standard protocol to help prevent me from developing preeclampsia towards the end of my pregnancy. The long and short of why they don’t want people to develop preeclampsia is that it’s the last step before a woman can develop eclampsia, or having a seizure in pregnancy. And as I’ve been told more than once in the last 5 weeks – mommas don’t like seizures and babies don’t like seizures.
Even saying the word seizure makes me cry. Even now. Even with her here, next to me making sweet coos and grunts.
So back to Friday – the OB I saw that day was shocked and I think saddened I was continuing to work during this. She said your blood pressure is terrible enough as it is, and if work is stressful and your numbers get worse – your baby may have to go to the NICU. And that’s not worth it to me so I’m pulling you out of work as of today. This was only two days prior to when I was planning to leave work, after all my induction day was scheduled for next Thursday. My plan was to work Monday and Tuesday, tidy up the logistics of leaving work for a while, and then spend the day Wednesday and Thursday getting as ready as I can to be admitted Thursday night to have a baby.
But knowing I didn’t have to go back for those two days really made a difference in my stress level. Not that I didn’t want to work or help with the transition, but my body was physically done. I cried on the way home from work the day before that appointment. I cried because my body couldn’t move as fast as I needed it to find answers to my questions. I cried because my lungs were so fatigued that trying to explain things to patients took all the energy I had. I cried because my head hurt and it hadn’t stopped hurting since Dec 23.
So I went into the weekend with a newfound peace. A new grace and permission for myself to rest and prepare for this adventure. An adventure I knew nothing about. An adventure everyone around me told me was life-altering and amazing – but it’s just something you can’t explain or transfer to someone else.
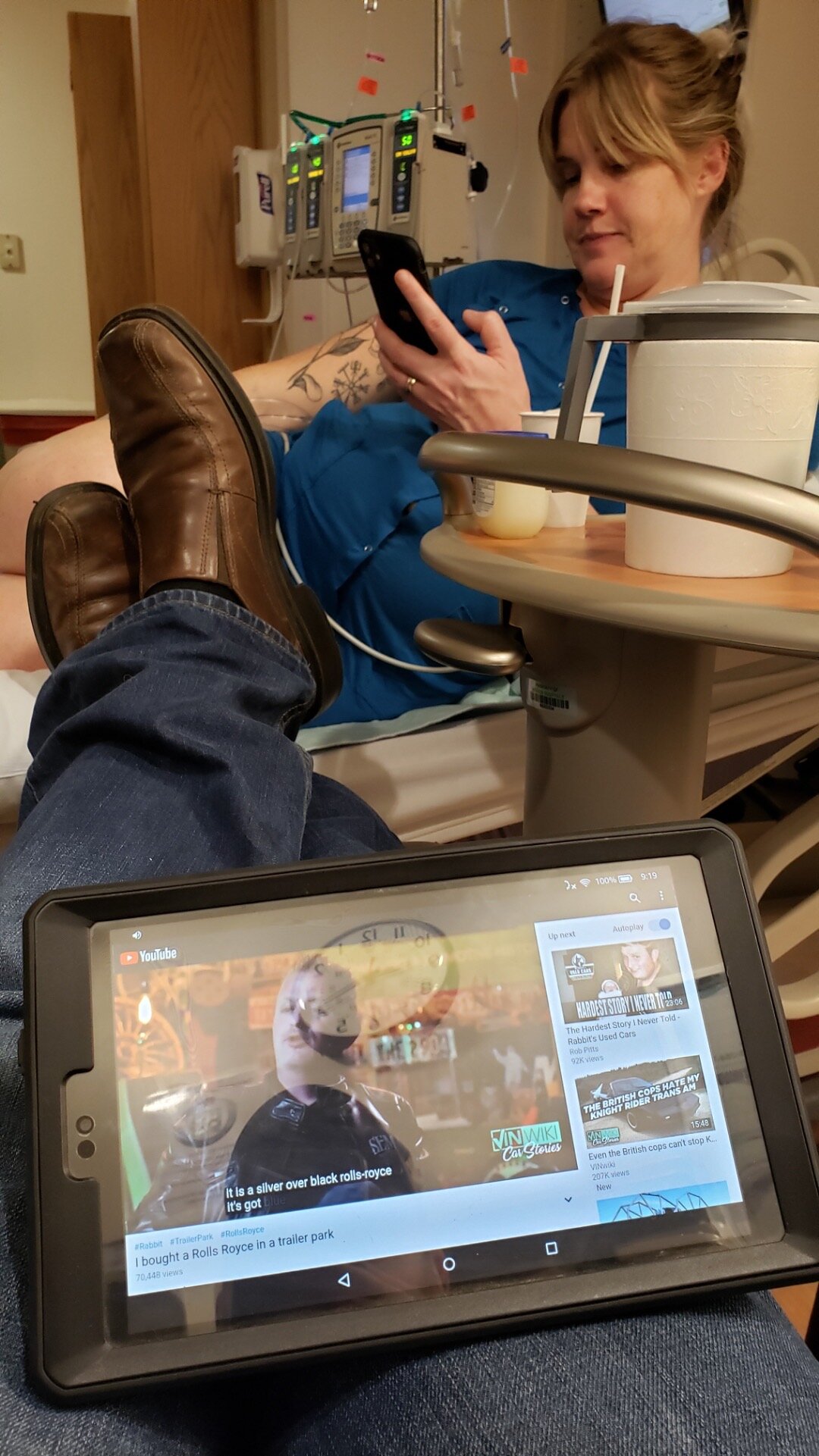
After dropping off the note at work saying I no longer can be at work I picked up Domino’s pizza and headed home for our last weekend as non-parents. We watched YouTube videos and hung out together as we had many nights before. The way I’d been feeling left me with little energy to do much in the evening.
Preparing – Whatever That Means
Saturday was the day we were supposed to attend an all-day birthing class ‘boot camp’. Due to my procrastination, this was the only class available and I’d registered and paid for it back in November. But due to feeling so poorly, we decided to bail on the class and just cut our losses on the class fee. Instead, my stepmom came over to do a nice deep clean of our house. Since I was technically on a sort of ‘bed rest,’ I didn’t think I could manage cleaning the way I wanted to before going into hospital. My stepmom graciously said yes when I asked for some help and I’m so glad I did – she made our home feel like a hotel!
Saturday afternoon we went out to celebrate a friend’s birthday at a few breweries and had dinner. The birthday girl had a baby in December and two other women there were pregnant as well so babies and pregnancy dominated the conversations for sure. I loved watching the dads and dads-to-be swap stories and advice. As well as give each other shit of course.
I’ve paid for going out during my pregnancy. I would feel fine and well at the time – enjoy friends and gatherings – and would feel like a dumpster fire on Sunday. Early on it would look like severe nausea for most of the day. Later on, it felt like a massive hangover with headaches and fatigue.
That’s how Sunday started so I kept it easy and low stress. My girlfriends from work came over to drop off baby hand me downs and even paint my toenails (since I can’t reach them without holding my breath). We picked a bright pink as my ‘laboring color’.
Monday I did more of the same straightening and preparing – whatever that means. The nursery was put together, Ben had put the car seat in his car, the house was clean.
I didn’t do much ‘resting’ as I continued to feel so poorly. Lying on the couch mindlessly watching Game of Thrones was great for a few hours at a time, but the most restful part was not being at work. Ben did his best to help me out – cooked me food, did household chores – but mostly he was patient with me.
Patient with my tears. Patient with my fatigue. Patient with my anxiety. He’s the one person I can be completely vulnerable with, but it is still a challenge for me to open up. Still a leap of faith that saying the silly things eating at my stomach to him won’t bring judgment. So I say those things and I exhale. I allow him to share my fears and suddenly they seem less scary and less large. Because he is there with me.
Should’ve Stopped For Fries
Tuesday rolls around and I’m due for another twice-weekly OB visit to check our baby’s heart rate, check my contractions, blood pressure, and labs. As I said, my blood pressure was slowly climbing. At this visit, it was high enough the midwife called the physician on call at the hospital to get advice.
They want me to go to the outpatient labor and delivery unit at the hospital to get my labwork done and watch my blood pressure. They wanted the lab results the same day and so I had to go to the hospital to get this done. I was annoyed I had to leave the clinic, drive to the hospital, park in a giant parking deck, and walk to this unit for basic labs.
I should’ve stopped at McDonald’s first to get some fries.
Waiting on results…and hungry
My blood pressure maintained that higher level. My labs continued to be stable, but my blood pressure wouldn’t go down. And when I asked the OB what she wanted my pressure to be in order for her to let me go home...I knew I wasn’t going home.
The face of a woman who knows shit’s about to get real but she’s too tired to care
By about 2pm she decided to admit me to get this party started. She said waiting another 48 hours for my ‘scheduled’ induction wasn’t safe and not really necessary. I think her words were icing on the cake if I could make it to 37 weeks officially, but that my baby is doing really well and I was given steroids in the hospital in December to further help my baby’s lungs develop.
I was able to convince her to let me go to the cafeteria and get some food before going to the labor and delivery unit. After getting some food in me, I felt a lot more at peace with getting things going. I’d also sent Ben a long list of things to pack because that was the only thing I had left to ‘prepare’ – my labor bag and bag to stay in the hospital for a couple days. I had the baby’s bag packed so that was easy. But my bag...I’m still impressed he was able to get the majority of the things I asked for to me.
I’d also told him to take his time. The OB told me to anticipate a 24-hour induction process. That didn’t mean 24 hours of active labor, but a full day to convince my body we were shortening the natural delivery timeline. I told Ben the longer he could stay out of the stuffy, dry, gross hospital and the fresher he could be for me/us – the better. So he came over around 6pm – with Sonic in tow, God love’m.
Hanging out waiting on this labor thing to start
Last selfie as a child-free couple! Note the heating pad in place helps ease contractions
Magnesium Toxicity Sucks
By the time he got there, I’d been placed in a nice big room that even had a tub! A tub I couldn’t use because they were going to start IV magnesium to help reduce the risk of seizures. There’s that word again. And there’s the tears again.
I give patients IV magnesium all the time. Chemotherapy and side effects of chemo can deplete magnesium. I’d never thought of it having side effects, I now realize that’s because there’s a difference in replacing magnesium to a get to a normal level and inducing magnesium toxicity.
Magnesium toxicity makes you feel like you’re hungover. But, I already feel hungover, remember? So it was this nice compounding effect when they gave me a bolus (a big dose at once) and then starting a continuous infusion. I felt heavy-footed, light-headed, and the headache persisted. They gave me non-narcotic medications. They gave me a Coke to see if caffeine would help.
Nothing helped.
They had also placed a catheter in my cervix and filled a balloon with saline to apply gentle pressure and mimic my baby’s head making her way out. This “gentle” pressure wasn’t intolerable but was hard to ignore. It applied pressure to my cervix making me have mild cramps. It applied pressure to my bladder, so here I am with an IV pole giving me medication causing fatigue and weakness, hobbling to the bathroom every 15 minutes. And lest we forget my amazing belly beautifully in the way.
When they placed the catheter – around 4pm – I again was reminded the catheter can stay in place for ‘up to 12 hours’ and since this was my first baby, the odds things would last that long were greater. Around 8pm the OB came to check on the balloon. I was told the balloon falls out when you’ve reached 3-4cm dilation. But rather than falling out, the OB tugs on the string and sees if it basically will gently be pulled out. And pull out it did. I’d already reached 3-4cm after four short hours.
The anesthesia team interviewed me when I first got to the room about an epidural since I said I wanted one. They reviewed my records and risks. They warned and advised me that from the time I request an epidural, I will get one placed and feel the benefits of the epidural an hour later. This is to account for the team being paged, them arriving to my room, giving me a liter of fluid beforehand, carefully placing a needle into my spine, and infusing medication to numb me from the waist down.
Once the catheter was out, the OB said she would come back in a little while and break my water. I don’t remember how long ‘a little while’ was but it didn’t seem like very long. At this point, I was feeling contractions but they were mostly something I noticed and not something painful. It felt like my belly muscles were tightening rather than period type pain – at this point. It also felt like gas pains and I verified this by asking the nurse after having this gas-like pain if I was having a contraction. She said yep, that was one and I realized I’d been having contractions 3-4 times a day for the last couple days.
One Small Nick For Womankind, One Giant Leap Into Pain
Using a small tool, I wasn’t too eager to look at what kind, the doctor broke my water as I lie in bed. My nurse had half a dozen towels to catch what she could and save the sheets I was on. I didn’t feel anything when she broke it, but I did feel the warm rush of fluid running down my leg. Was like someone had poured warm water down my right thigh. She said the fluid was clear – which is a good thing. She also said she barely nicked the membrane and my water broke, signifying it was about to break any minute on its own.
At the time I didn’t think much of this moment, but now I can’t stop thinking about it. It was the first time anything touching her, was now outside of me. I felt the warmth pour over me like a sweet, gentle baptism into labor. It was also one of the last times I would feel anything below my belly button until a few hours after she was born so part of me really holds on to that ethereal experience.
Ok, you’re not going to like me in a few minutes…we are starting Pitocin now and your contractions are going to start to become more frequent and more severe said the OB as she cleaned herself up and the nurse helped clean me up from the watery encounter.
I’m glad she warned me.
The rate and intensity of my contractions started to increase steadily and quickly. I went from barely noticing them to having to stop talking to Ben and focus on my breathing to get through them. He was able to see the strength of the contractions on the monitor and would tell me how high they were going and then when they would start to level off.
Comfortably Numb
I called the nurse and said I’d like that epidural now. And I’m glad I did because in addition to all the things they normally do to get it placed, they also had to draw blood to check my platelets before they would place it. This is due to another issue called HELLP syndrome which is associated with preeclampsia. If you have HELLP, your platelets can be low, increasing risk of bleeding and complications from, say, putting a needle into your spinal canal. I didn’t have HELLP but the risk is greater if you have preeclampsia so they screen for both.
Thankfully the lab person came in quickly and drew my blood. Thankfully the CRNA who placed my epidural was very chill and clearly had done a few in his career. He walked me through the steps as he was doing it because I couldn’t see him behind me. Ben was able to sit in front of me as I sat on the edge of the bed bent over and hold my hands as well as distract me.
The lidocaine hurt the most. I knew it would. He told me it would. But it freaking hurt. Big pressure. Big burning. Lasting less than 10 seconds, like he told me it would. Then I had a contraction and had to do my best to be still during this next part – the threading the needle part. My right leg quickly went numb.
Then I felt like I was going to puke everywhere.
An anticipated side effect of epidurals is a fairly sudden drop in blood pressure. They try and compensate for this by giving you that bag of fluid before in your IV. But my blood pressure still dropped and I immediately felt nauseous. They quickly laid me down on the bed to try and offset the pressure shift which kind of helped. The interesting thing was my blood pressure was now in a normal range for the first time in four weeks. But it still made me feel awful. And it made my baby not feel good either. The OB said even though my blood pressure is now ‘normal’, my baby was used to it being high just like I was and based on her heart rate and other nuances they look for, she could tell that my baby wasn’t really enjoying the drop either. So they gave me more fluid through my IV to help both of us feel better.
Since my right side was numb and not my left, they needed to fix this. They put me on my left side to have gravity help move the medication. This helped a little but I still had sensation in my left lower belly which created very pinpointed contraction pain. He then either gave me more medication or a different medication and eventually, both sides were numb.
My reasoning for wanting an epidural was multifactorial. I’m also aware I didn’t need any reason at all to want one. If I wanted one, no explanation was needed. But for the sake of labor stories – I’ll elaborate on one of the bigger reasons. When I lived in Alaska I had a pretty epic four-wheeler accident which resulted in me fracturing and dislocating my tailbone. The end result of that injury was pretty persistent sacral pain as well as the tailbone itself becoming more tucked underneath me.
I went to pelvic physical therapy in Alaska as well as North Carolina to address pain and mobility issues and made a lot of progress over the years. I was in a good place when I became pregnant – a place that slowly transitioned into a not so good place. With all the natural Relaxin flowing to help relax my pelvic floor to accommodate a baby in there as well as prepare for birth – the tense and stressed muscles around my tailbone did not move. To me, it felt like when an iced-over river or bay starts to break up and flow but there is one area that won’t thaw, budge, or move.
This stubborn area led to my severe pain returning. Sitting, squatting, doing basic bodily functions all became tender and sore. So the thought of pushing a baby past this area unmedicated was something I didn’t want to experience. Something I didn’t feel I had to experience to make my labor special.
Ok, so epidural is working, I am sufficiently numb from the waist down and can’t move my legs. The nurses helped reposition me on my side with this giant pillow called a Peanut (because it’s shaped like a peanut) in between my knees to help my pelvis open. I can no longer feel contractions at this point and I can’t feel my tailbone. I was actually really comfortable. I was 5cm dilated.
The green barf bag weil within reach
It’s now 11pm.
Being comfortable is a good thing because the plan was for me (and Ben) to get a few hours of sleep if we could in anticipation of going into active labor sometime tomorrow. Another nice thing about the epidural was I couldn’t get up and go to the bathroom anymore. It’s nice because the magnesium was making me so heavy feeling, getting up and down was becoming more of an issue and definitely interrupted any aspect of rest.
Instead of me going to the bathroom, they would place a catheter to drain my bladder every 1-2 hours. I’ve placed many urinary catheters as a nurse and they aren’t the most comfortable thing to have done – but thankfully I was numb down there! So I felt nothing when they did this.
Calm Before the Storm
Once my bladder was emptied and I was positioned on my side, the OB team left us be for an hour or so. I was heading to sleep when the nurse and the doctor come in. Again, being a nurse, I know if both members of a team walk in – unscheduled – there’s something noteworthy going on.
My baby’s heart rate was dipping down when I had contractions. They knew this because the monitors on my belly are showing up on a screen at the nurse’s station in the hallway. This correlation indicates the baby is under stress. In their words, the baby doesn’t like the position you are in...so we are here to move you. Together they rolled my 5ft11in, 221lb body to the left side – peanut pillow and all. And left again for us to rest. It’s now approaching 2am.
A few minutes later, they’re both back. Your baby doesn’t like being on this side either.
Slight side note here on this statement. Throughout all the complications I have had during my pregnancy from nausea, fatigue, dizziness, and progressing to hypertension and migraines – my baby was always described as that’s one happy baby!, beautiful readings, her heart rate looks gorgeous. Every single time. Every time we went in to check on me and her – she was always thriving and doing great. Every time I was so grateful to hear it.
So to hear that shift to “your baby doesn’t like this” was more than a little distressing to me. It was at this point the OB said she wanted to place an internal monitor to get a better idea of how my baby was doing. I don’t really know what else they can see on the internal monitor but I was glad to get a literal closer look at her and her status.
The doctor had the monitor in her hand and began to insert it. Then the doctor said Oh, hello. Ok, we’re having a baby. Like right now and we need to start pushing.
Um, excuse me?
I was now 10cm which is fully dilated. My baby’s head was pushing against the OB’s hand at this moment. She then called out for the nurse to go in the hallway and “grab everyone” according to Ben. I said to Ben – call Roxy RIGHT NOW.
Roxy was our doula. She was someone we had met a few times along our pregnancy to help create a plan and to be a support person. Doulas are a group of birth workers who provide many types of support to pregnant people and couples. Roxy came highly recommended by a few friends and I thought having someone there in the room with Ben and I would be helpful.
Hospitals and procedures, needles and blood don’t bother me. I wasn’t scared to be there. Even my day shift nurse said she could tell I was ‘something’ meaning something medical. She said I had a slightly authoritative vibe and was entirely too calm for the current scenario at hand. But having someone who was there to not provide medical support – someone there to provide emotional support to me and Ben was important to me.
Someone to be there since my mom couldn’t.
Roxy had been in close contact with us since I was admitted. We’d talked on the phone a couple times that night and texted a fair bit too. Based on her experiences it would be a while before I went into active labor, so our plan was for her to come around 6am Wednesday morning. After all, I was only 5cm at 11pm and people can hang out at this step for a while – especially first time moms was what the OB said.
Clearly my baby is an overachiever already. Ben calls her and tells her Hi, uh Steph is about to push and have the baby… and Roxy was quickly on her way.
In about 2 minutes, we went from a dark room with me, Ben, doctor, and my nurse to the brightest lights I’ve ever seen, 2 additional NICU nurses, and 2 additional labor and delivery nurses.
In about 2 minutes, I went from lying on my side covered up in blankets to my legs hoisted in the air wide open in stirrups that magically appeared out of the bed. Ben was near my left shoulder closely watching me and everyone else.
Pushing...
While everyone was getting stage ready, the OB is talking to me. She tells me she needs me to start pushing very soon. This was when I briefly thought shit, I should’ve taken that class, I have no idea how to push.
She either read my mind or I said out loud I don’t know to push because she said, bear down like you’re pooping, and push until I tell you to stop, that’s all you need to do. So that’s what I did. I exhaled while I pushed and she told me to hold my breath next time. So that’s what I did the second two pushes.
People told me pushing is harder when you have an epidural because you can’t feel anything down there. I always found that hard to understand because if you all of sudden couldn’t feel your butt, it’s not like you forget how to poop? I learned the real issue is I needed to push while I was having a contraction – and thankfully – I couldn’t feel them anymore. What we did to mitigate this lack of deep sensation was: I focused and tried to feel any sort of pressure shift in my belly, OB looked at my monitor to measure them, and my nurse had her hand on my belly to feel them. By using these three gauges, we were able to roughly tell when they were happening.
I pushed three times for every contraction. The OB said I was a strong pusher. Now, no one will ever know except for her if I was actually a strong pusher, but I do know I felt like my head was going to explode and Ben said the veins on my nose were popping out. My heart rate and blood pressure were also spiking during each push, but I can’t imagine they wouldn’t in anyone birthing a human.
Falling in Love with Him All Over Again
The nurse told Ben to hold my leg and so he did. The nurse told Ben to hold an oxygen mask over my face in between pushes and so he did. When we met with Roxy to discuss birth preferences I said I liked music and would like it during labor. So before I started pushing, Ben started playing Mumford and Sons Pandora on his Kindle. He offered me words of encouragement and support. Looking up at him I could see his attentive eyes and face watching everyone and me – doing his best to be our protector. I say ‘our’ because he’s had two people to worry about this whole time. Me and our baby. Two lives he feels responsible for protecting. And he wasn’t going anywhere.
I laughed when I was admitted because there is an ammonia packet taped to the bathroom door. Clearly smelling salts for those who pass out witnessing labor...Something I knew Ben wouldn’t need. He was there in it for us.
Say what you will about medicated labor, but I will always be grateful to be as present as I was in those moments. To listen to the doctor guiding me through pushing. To listen to her ask Ben can you see her head? Come see her head, she’s making her way out. To listen to Ben talk to me and watch him become a father. If I had been incapacitated with pain, I don’t think I would’ve been able to take all of those sweet memories in.
Almost There
After about 10-12 minutes of active pushing, our baby’s head was making her way out. Her heart rate was still dropping when I pushed – again signaling stress. It was at this point the OB asked if she could use a small vacuum to help guide her head out. She said she had no doubts I would birth this baby very soon, but she wanted to get my baby out of this position ASAP. I said yes, I wanted her to come out quickly and get out of distress.
The OB said 3-4 times that the vacuum did not replace pushing and I had to keep pushing as hard as I was to get her out. So that’s what I did. Three more big pushes and two ‘smaller’ ones (to reduce the amount of tearing for me) later, at 0251am, I heard the most glorious sound I’ve ever heard.
My baby’s voice.
She came out crying immediately. Something I was so very hopeful for. I didn’t want to experience a millisecond of pause for them to have to arouse her to cry. The OB pulled her out and handed her to the NICU nurse standing on my left side, next to Ben. The nurse essentially threw Aspen on my chest for us to see her, all while suctioning out her mouth as she cried out announcing her arrival. She cried and I cried. Ben cried. I was awestruck. Her face. Her dark hair. Her voice. It’s still difficult to comprehend. I felt like I was in a movie or in someone else’s body. There’s no way I made such a beautiful and loud little baby.
60 seconds later, the OB told Ben to cut the cord. And so, he did.
A New Patient Is Now In the Room
After a few moments embracing our first encounter as a family of three, the NICU nurses took Aspen to check her out. They had a little baby warmer, affectionately called the Panda something...and did her vitals as well as APGAR scores. According to Ben she was acing all the checks. She was only 5-6 feet away from me but I was thankful Ben could be there with her and relay the information.
As far as me, the OB was slowly working on removing my placenta. I think I pushed a couple of times, but it was more of her gently tugging and massaging my belly to get it down. Once it was out, she placed it in a bowl on a table next to her. I wanted to look at it so she held it up in the air. I’d become fascinated with placentas – how they form, what they do, the fine balance with our bodies. I’d created an organ made of 50% of Ben’s DNA, how crazy is that? They also say the placenta is thought to be the root of preeclampsia which furthered my fascination. This bloody jellyfish looking organ kept Aspen alive all while trying to overtake me.
How bad did I tear? was my next question. She was cleaning me up and removing blood to get a closer look. She said I had a stage II, or mild tearing and the tearing wasn’t near any major openings. I also tore around my urethra which I for some reason never thought about tearing up – all the horror stories talk about tearing down, near your rectum, and all the issues that can happen from that. So that was new to me, and would also be the more painful area in the hours to come.
She stitched me up – again thankful for my epidural because I felt none of it. They put the urinary catheter in me again to drain my bladder. The nurses cleaned up the OB, cleaned up the floor, and cleaned up me. I never saw any blood, other than the blood on Aspen when she came out, but Ben said it was an impressive volume of blood loss.
Once she was sufficiently checked by the nurses, they handed Aspen back to us for some skin to skin. They laid her little body on my naked chest and again my heart exploded. It was the first time looking at her face, her tiny squished face covered in vernix. She was quiet. She hadn’t cried out since that initial beautiful announcing cry into the world. She was sleeping peacefully on my chest with her dad watching over us closely, standing again over my left shoulder.
A Doula Walks into a Room
Remember Roxy? This is when she walked into the room. She didn’t see Aspen at first, after all, she was only 5 pounds 11 ounces and 18.5 inches long. Roxy comes in, sees my legs in stirrups and greets us all. She’s mentally preparing to help me labor.
Oh my god, there’s a baby! and we all started laughing. Since she lived outside of town, like we did and many others, it took her a little while to get here. Since Aspen is an overachiever, we were only in active labor for about 15 minutes. So from the time Ben called Roxy to when we met Aspen for the first time – it wasn’t really enough time to park and walk into the giant hospital.
Even though Roxy had missed our actual labor, her role in our story was still very needed. The time she spent at our house just a week prior going over preferences for both of us, asking questions we wouldn’t have thought to ask, bringing up scenarios we didn’t know to think of – helped us in her absence. Ben knew what I wanted based on that meeting so he filled that role. He had a better idea of how to support me based on Roxy being part of our birth story and that is worth it all to me.
So now Roxy was here, she was checking in on both Ben and me – as well as enjoying Aspen with us. She helped me try to get Aspen to latch on – which she did! Although it was brief. But the proof of concept – the proof that I made this baby, I have these boobs, and the two may work together – gave me so much hope in that moment.
After a few hours, we were transferred to the Mother/Baby unit. So during my pregnancy, I’ve spent time in three units – Maternal/Fetal the week of Christmas, Labor and Delivery, and now Mother/Baby. Roxy helped wheel my IV – yes the magnesium was still going and was going to continue running until 24 hours after birth. So I was stuck with an IV pole and magnesium toxicity symptoms until roughly 3am tomorrow. Ben is pushing the cart with all of our stuff on it. The nurse is wheeling me to the room. I am holding Aspen. I shakingly was able to transfer from the bed to the chair with a lot of assistance.
It’s now around 6am and we are all exhausted. Roxy holds Aspen for a while so Ben and I can take a small nap. After some more latching guidance and a hug, she heads out to allow us some time as a brand new family of three.
First Day Together
Throughout the next day, my dad and stepmom come and visit as well as bring us some much needed breakfast. Later in the day Ben’s parents arrive after traveling a few hours from their house.
In between visits from the new grandparents and my niece, we meet a pediatrician and the new OB on call stops by to check on me. We also have a great nurse who helps both Aspen and me throughout the day. I’m still not producing much by way of milk, which is an expected response, but the concern is Aspen hasn’t really eaten anything yet. And since she’s small and technically pre-term, they were watching her blood sugar levels closely. They were low, but not dangerously low.
My nurse said even a droplet of colostrum (the nutrient and fat-rich breast milk that comes in first) would help her blood sugar. I thought she was mostly being encouraging but it did help. We were able to get 1-2 drops onto a plastic spoon and drop them into her mouth. Her blood sugar responded with that and from there on, she maintained her levels wonderfully.
Another thing they were watching closely was her temperature. Since she didn’t have as much ‘brown fat’ on her, she had to work harder to stay warm – working hard burns calories and can make blood sugars drop. So we did our best to keep her bundled and do skin to skin – both Ben and me.
Skin to skin <3
Once a little more milk was coming in, we were taught how to feed her with a tiny plastic syringe. I had no idea this was a thing – feeding newborns like baby goats. But since she’s small and worn out (the IV magnesium I was getting prior to delivery was affecting her too), we had to help make feeding as easy as possible. Ben became a pro at this and I’m so thankful he had that time to build a bond with her by feeding. He would put the tip of his finger in her mouth and once she started sucking, he would slowly squirt the milk in with a syringe.
He even got fancier and they gave us a tiny tube to attach to the syringe and he taped it to his finger. As you can see, he was a professional and Aspen is locked in on him.
Tears of Joy and Pain
We spent many moments that day in tears over the enormity of what had just happened. Tears over how perfect she was and how thankful we were to finally meet her. I also spent time in tears because I still felt terrible.
Yep, the whole your pregnancy symptoms magically disappear when you give birth worked for the nausea and heartburn, but my blood pressure was still elevated and my head still killed me. I cried in frustration about how I couldn’t fully enjoy Aspen because I felt so awful. I cried that Ben still had two people to take care of and we couldn’t just focus on Aspen. The staff told me it was probably the magnesium, but the symptoms were so similar to how I was feeling pre-labor, I had hesitations.
Thankfully within a couple hours of turning off the continuous infusion, I was so much better. Ben said you’re finally you again as I was puttering around the room, cleaning, taking a bird bath, and changing clothes at 6am. I finally was free of a headache and the heavy-footed/hungover feeling had faded.
My blood pressure was still elevated so they started me on an oral blood pressure medication. They eventually had to increase the dose because they didn’t like how high it was staying. They checked it frequently and told me to ‘relax, chill out, think calming thoughts’ when they checked it. Which is really hard to do knowing if the numbers aren’t what they want – I couldn’t go home with my baby.
It’s also hard to be calm and relax when you’ve been instructed to feed Aspen on a 2-3 hour schedule. Feeding her meant we had to:
Wake her up (we had to learn how to wake up a baby after spending months reading about how to get your baby to sleep)
Try to see if she would latch
Heat up previously pumped milk and syringe or finger feeding it to her.
Pump since she’s preterm and isn’t going to ‘demand’ from my breast like she will a few months from now and it’s all about supply and demand people!
Wash the supplies in the bathroom sink because I only had one set
Pile of pumping and feeding supples
And then try to sleep? Eat? Take a sitz bath for my ripped perineum? Stare at my perfect baby?
Thankfully my blood pressure was stabilized at the higher dose of medication and we were scheduled to escape on Saturday after spending an extra day in the hospital.
Going Home
Here we are – the morning of discharge. The nurse goes over a long list of things to watch for – one list for me and one list for Aspen. Ben had the car seat in the room and the nurse shows us how to get her inside safely. Since she was so small it really swallowed her up but we were able to get the straps nice and snug for me to feel like she wasn’t going anywhere.
Ben goes and gets the car and we meet him out front. I’m realizing I hadn’t left the hospital room for 4 days when I can barely walk down the hall to the elevator. Up until this point, everything with Aspen was inside a hospital, using hospital things. She wore a cute hospital hat, and the only clothes she wore were a diaper and swaddled with the blue and pink hospital blanket – you know the one.
But now she was wearing clothes (which swallowed her as well) we had picked out. She was in the car seat we registered for. She was in Ben’s car. And we were taking her home. I could sigh with some relief. Because that anxiety I mentioned at the beginning was highest in the hospital. I felt the least in control while we were there. And now we are on our way home with her.
The first day home was hard. And not even really to do with taking care of her. She’s made that the easy part. Feed her, supplement her, pump, change her diaper, bundle her up, watch her sleep. Easy peasy. Processing what had just happened to me and her and Ben in the last week – that was a different story. Pile on top that I was given explicit instructions to monitor for worsening signs of preeclampsia which could land me back in the hospital. Yep – not only can it persist, but preeclampsia can get worse postpartum.
Those first few days will likely make their own blog post as there was so much going on and to process. As will a post about my pregnancy.
But for now, meeting Aspen has been the most life-altering thing I’ve ever encountered. And if you know me, I’m not one for absolutes. There are rarely the best, the most, the worst thing in life, there’s a lot of gray areas. But I can say without hesitation, meeting Aspen and bringing her home has categorically changed me and its the most beautiful and terrifying thing I’ve ever experienced.